Long Haul Syndrome (aka Post Infection Syndrome)
There is no doubt that COVID-19, and everything it brought, changed all of our lives in drastic
ways. For some people infected with SARS-CoV2, they may still be feeling the physical effects,
even up to one year later. This is what has recently been dubbed “Long-Hauler Syndrome.”
Classically, however, it is known as Post Infection Syndrome.
So, what is it? Some describe it simply as a “blah” feeling, while others describe it as
soul-sucking fatigue. You feel like you are on this hamster wheel — never feeling as bad as when
you were sick, but also never feeling like yourself again. Post Infection Syndrome has been
recognized for decades; however, it has been poorly studied and scarcely mentioned,
oftentimes being diagnosed and treated as other syndromes with similar symptoms.
Top 3 symptoms of Post Infection Syndrome:
Fatigue/Brain fog
Depression
Weakness/Achiness
Many of these symptoms have a clear laboratory track record and can be detected by your
doctor via thorough questioning and lab diagnostics. Worth noting is that fever is not usually
found once the acute infection has passed. In fact, we will commonly find slightly lower than
the patient’s normal temperature in the post-infectious phase.
Clues for Diagnosing Post Infection Syndrome
Developing a timeline of symptoms with your doctor is critical. The first thing to rule out may
seem rather obvious, but I can tell you that it is largely overlooked or dismissed. We must first
determine if the infection has cleared. Most infections will last a couple of days, up to a few
weeks. However, certain pathogens we classify as persistent. Persistent infections can last
months, if not years. Although all classifications of infections (bacteria, fungus, virus, parasite)
can persist past a few weeks, viral and fungal pathogens are most notorious for sticking around
longer.
Cortisol Levels
Once active infection is ruled out, we must then investigate the downregulation of the immune
response. Cortisol is an important part of the story when we discuss Post Infection Syndrome.
As the primary stress hormone, Cortisol serves an immunomodulatory role: in essence, helping
to regulate the immune response or “quiet it down” when needed. Without it, our immune
system would run wild, chewing up gobs of energy and leaving destruction and inflammation in
its wake. Under normal circumstances, cortisol will be released to calm down the immune
response after infection and return it to its resting state. The body then repairs and regains
what was lost and it is ready to fight another pathogen.
Some infections, however, directly affect cortisol release. In these instances, cortisol is released
in such high amounts or for such prolonged periods of time, that this exposure causes the body
to react abruptly. The brain will register the excess amount or prolonged length of cortisol
production as “inappropriate” and attempt to compensate by shutting down cortisol signaling
altogether. The triggering of this feedback mechanism may continue, causing cortisol levels to
drop very low, and resulting in sugar imbalance, fatigue, and blood pressure dysregulation.
Cortisol depletion is a very common finding in patients with Post Infection Syndrome and is
the centerpiece of Long-Hauler Syndrome.
Oxidative Stress
Infections also induce substantial amounts of oxidative stress, requiring a corrective compound
to counteract the damage. Enter: antioxidants. Antioxidants are normally consumed at a
relatively constant rate in the average diet (think colorful vegetables and fruits) and are recycled
when other vitamins and minerals are balanced. There must be enough of these nutrients
on-tap to handle the higher load of oxidation, post-infection.
Anorexia (loss of appetite) is commonly found during an acute infection. For a short period of
time, this may be an advantage. Fasting can improve short-burst immunity and promote cellular
turnover. Not to mention, the lack of food consumption guarantees the patient is not
consuming anything that could halt the immune system (sugar) or put more stress on it, such as
in the case of food sensitivities.
If decreased appetite lingers for too long, however, the patient becomes nutritionally and
calorically depleted — leading to “antioxidant debt” and mineral deficiencies. Increased damage
results from the body not having these resources to repair itself. The patient is then stuck in a
constant state of catch-up.
Cellular Integrity
In prolonged inflammation, fatty substances are used to communicate within the immune
system and the body must find a reservoir to acquire them from. We have a massive store of
these fatty substances in our cellular membranes, so our body will cannibalize the integrity of
our cells to continue the immune/inflammatory process. Cells weaken and are unable to freely
pass essential information across the membrane, eventually bringing about poorly functioning
cells and increased cell die-off. The result: more mess for the body to clean up.
Now what?
A variety of other diagnoses must be ruled out before arriving at a clinical conclusion of Post
Infection Syndrome. Like with any medical condition, we must get to the root cause of the issue
and work our way forward with the right map, rather than aiming at symptoms in the dark. The
best place for patients or clinicians to start is by recording a timeline of when symptoms
occurred and their correlation to the infection. From there, a series of specific tests should be
performed by your doctor, in order to guide accurate decision-making and treatment
recommendations.
Post Infectious Syndrome can be rather complex, and we only scratched the surface here.
However, as we continue to work with patients before, during and after SARS-CoV2 infections,
we are encouraged by some of the positive outcomes we have seen at our clinic!
- July, 01 2021

Please wake up with 10 fingers on July 5
Independence Day is a celebration of the United States of America. After all of the...
- March, 12 2021

Tick Tock – Daylight Saving Tim...
What do the states of Arizona and Hawaii, along with Puerto Rico, Guam and the...
- July, 22 2021

First cases of West Nile Virus detect...
The first positive West Nile virus mosquitoes have been detected in Larimer County this year....
- December, 18 2020
Larimer County Not Yet Eligible for S...
The Colorado Department of Public Health and Environment announced the "5 Star Certification Program" this...
- May, 13 2022

May is National High Blood Pressure M...
May is National High Blood Pressure Month. This is the month that is set aside...
- July, 14 2022
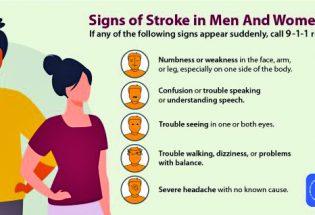
Risk factors for stroke, including th...
Adults from all walks of life likely know at least one individual who has suffered...

Unified basketball comes to Turner Middle School
Community News
Mike Grace says goodbye as Brett Wing joins town board
Community News
POLICEBLOTTER
Community News
Northern Water sets C-BT quota at 70% for 2024
Community News

Emotions run high during Revere Property hearing
Community News
Snowpack at 119% above normal
Community News

Karspeck to serve third term as Berthoud mayor
Community News
COMMUNITY CALENDAR:
Community Calendar – add an event
Homestead Fine Art Gallery First Fridays OPEN HOUSE
03 May 4:00 PM - 7:00 PM
Homestead Fine Art Gallery First Fridays OPEN HOUSE
07 Jun 4:00 PM - 7:00 PM
Homestead Fine Art Gallery First Fridays OPEN HOUSE
05 Jul 4:00 PM - 7:00 PM
Homestead Fine Art Gallery First Fridays OPEN HOUSE
02 Aug 4:00 PM - 7:00 PM
Homestead Fine Art Gallery First Fridays OPEN HOUSE
06 Sep 4:00 PM - 7:00 PM
Homestead Fine Art Gallery First Fridays OPEN HOUSE
04 Oct 4:00 PM - 7:00 PM

